This week on the Dental Up podcast Shaun Keating (founder of Keating Dental Lab) and Bob Brandon GM Talk Implant Solutions.
Full Transcription:
Shaun: Hey everybody, Shaun Keating here. Like to welcome you to this week’s Dental Up podcast. We’d like to welcome Bob Brandon. He’s our general manager here at Keating Dental Lab. Bob, how you doing?
Bob: Great. Thanks for having me.
Shaun: Good to see you, man. You know, this week, we’re going to talk about implants and the best practices when it comes to implants. A lot of dentists are taking up placing implants right now, or they’re sending them out to maybe an oral surgeon, but, so we’re going to talk about different ideas, what we see, what we recommend, and how to make your life a little bit easier when you’re working with a dental lab when it comes to implants. First, I’d like to start off with some sports. Bob’s a big sports guy.
I know your little guy’s into soccer and all that. I’m not a big soccer guy, but oh, well, no, but football, did you watch a little bit of Pro Bowl yesterday? That thing was boring, man. NFC kind of, I think the highlight was Ezekiel chasing a fan that ran onto the field.
Bob: Yeah, that was crazy. I did see that.
Shaun: That’s interesting.
Bob: That was about it, though.
Shaun: I know. It’s like, it’s kind of crazy, you watch this game … I remember, I like it better with the format where it’s the week before the Super Bowl instead of the week after.
Bob: Yeah.
Shaun: I like it better in Hawaii, but it’s like, on the very first play, they have a run or whatever, and it goes, and everyone kind of just stands up, and it’s like they hug, and it’s like …
Bob: They don’t want to hurt each other.
Shaun: What the hell? Freaking hit them. The guys that are just, it’s like, it’s not even a real game. It’s like patty cake, man.
Bob: Yeah, yeah.
Shaun: It’s like, and I know, yeah, the season’s over. Guy, you’re going to get injured, you’ve got eight months to rehab, you know? I think I read somewhere, like, if they paid the guys a reasonable amount, like their salary or something, they might play harder, or maybe not, but I just don’t think it’s ever going to be a great draw if they’re not going to be playing a hundred percent.
Bob: Yeah.
Shaun: Play the game.
Bob: It’s a glorified all-star game.
Shaun: Yeah.
Bob: It’s just one step up from flag football, really. They don’t want to get hurt. They don’t want to hurt their friends. They don’t want …
Shaun: Yeah.
Bob: You know, it’s, it is a big risk. You got to understand it from the owner’s perspective, too.
Shaun: Yeah.
Bob: You don’t want your key guys missing a lot of time …
Shaun: That’s true.
Bob: Because they’re injured.
Shaun: Even like in baseball, you’ve got some of the guys that sit out because they’re in, you know, a race or whatever, and it’s only halfway through with baseball, but they even kind of, but they still, you know, they can hit the ball hard as they can and all that. I think I’ve seen one play where one of the running backs, I forgot who it was, got really freaking nailed, and he got up all pissed, like, “What are you doing? You hit me.” It’s like, “Well, it’s about time someone freaking hit you.”
Bob: It’s still football. At the end of the day, it’s still football.
Shaun: Ah, but it’s just like, I’m just bumming, thinking about, you know, another, I mean, it’s great Super Bowl’s coming up this week, but then after that, it’s like, fuck, I mean, you know …
Bob: Yeah.
Shaun: You’ve got baseball, and you have basketball.
Bob: I don’t watch any of those …
Shaun: Yeah.
Bob: That’s for sure.
Shaun: I mean, it’s not as exciting, but you know, we’ve got March Madness. I love college basketball, really, when it comes to March Madness, you see kids playing for the love of the game, and not for the money. Basketball, you know, Lakers …
Bob: A lot of your customers love your March Madness pool.
Shaun: Oh, yeah.
Bob: Right?
Shaun: We’re a sponsor of March Madness pool on Dentaltown every year, and I think it’s up to about five grand.
Bob: They like you for the money.
Shaun: Yeah. Well, it’s like, but it’s always better when you’re like, you’ve got something to play for, I think. I always like it. It makes it a little more interesting, even after, I think, after we get all the people that are out of it, after 99% of the people out of it, when it’s down to the last few guys …
Bob: Yeah, in the money rounds, yeah.
Shaun: We do something where we add in, okay, give us the total score of what it’ll be, so you’ve got a chance, and, you know, we’ll throw 500 bucks or something, closest score to the final, you know, or whatever, and so you’ve got some hope of something, but what about, did you see any of the horse race? They had a big horse race on Saturday.
Bob: You know what? Unfortunately, my weekend was all little guy’s soccer, unfortunately. I missed everything this weekend.
Shaun: I talked about it last week on our podcast. I’m a big, not a big horse guy, but I like, you know, watching the favorites and betting on the favorites and stuff like that. They had the Pegasus, which, I thought it was in Abu Dhabi or somewhere, but it was in Florida.
Bob: Oh, wow.
Shaun: I went down to my little local place, Sammy’s, and my wife went with me, and you know, California Chrome is always, I bet on him every horse race, and I’ve won almost every race except like the last race. This time, I didn’t bet him. I bet on Arrogate, and my wife bet on, you know, she put a little money down on California Chrome. I almost went California Chrome, because I’m like, “Dude, I really feel this, he’s going to come back and win this race,” but then in my gut, you know, you bet with your kind of, try to bet smart, so I went ahead and put the money on Arrogate, and lo and behold, man, that damn horse …
Bob: Awesome.
Shaun: Went and smoked everyone. I think California Chrome took like tenth.
Bob: Oh, jeez.
Shaun: Just horrible, and so now, I hear, I guess there’s a little knee issue, might be a little chip in the knee, and he’s off to stud fees now, and I think he gets $40,000 a pop.
Bob: Wow. Well, hey.
Shaun: What a good life.
Bob: It’s good money if you can …
Shaun: Go have sex, you get 40 grand, or to go mate with a horse, whatever you call it. Whatever. Thank you Arrogate. I got a pocketful of money from you there, and …
Bob: Awesome.
Shaun: Yeah, it’s kind of crazy. I just, I’ve been really lucky, but I, it’s not real tough when you just kind of bet on the favorites.
Bob: Yeah.
Shaun: You know, I’m not really good on trifectas or, you know, a exacta, you know, those are tough.
Bob: Yeah.
Shaun: Then, you can do that sometimes when when you box it. You know, you can box, say, “Okay,” you know, “This horse and this horse, first or second, either way,” but it costs you double the money.
Bob: Sure. Yeah.
Shaun: I don’t think you get as much, but other than that, you know, what else do we have? Any other sports?
Bob: You’ve got signing day for college football. That’s Wednesday, so that’s like a national holiday for a lot of people. That’s when, you know, the school’s will get restocked for, you know, the years to come.
Shaun: Alabama will get all the best players, and all the others sign … It’s kind of crazy.
Bob: Yeah, it is crazy.
Shaun: Then Harbaugh in Michigan. I mean, I just love, every college game in football this year, if I could see Michigan, I would watch it, because he’s just a great coach, and those guys were nothing a year or two ago, and he’s, with a bunch of scrappy players, and not a bunch of great recruits …
Bob: No.
Shaun: He’s delivering a pretty damn good team, and give him a couple years, I think, with some good solid recruiting classes, I think they’re going to be up there in the one to twos every year, you know, just because he’s a great coach.
Bob: Yeah. Got to beat Ohio State, though. You’ve got to get past Ohio State …
Shaun: Oh, I know.
Bob: If you want that end result for Michigan.
Shaun: Can you believe that? That’s just unbelievable, but …
Bob: Yeah.
Shaun: Yeah, but other than that, we had a pretty slow weekend when it came to sports, other than some horse racing and a little bit of NFL, but next year, next week’s the Super Bowl. Who do you like for the Super Bowl, Bob?
Bob: Man, you know, my heart says Patriots, but I’m hoping the Falcons win.
Shaun: I don’t know. You’re a Boston guy. You went up to, you went to dental school up there a little bit for a few years back in the day …
Bob: I did, but luckily, when I was there, the Patriots were horrible, so you could actually, the regular guy could actually get tickets and go see a couple games. It was actually before they even moved in to their new stadium, so …
Shaun: Oh, okay.
Bob: It was at the old, I think was called the Foxboro Stadium.
Shaun: Foxboro.
Bob: Yeah.
Shaun: What a trip. Yep. I remember we used to always go the dental shows. It’s called the Yankee Dental Convention, and actually, it’s …
Bob: It was last weekend.
Shaun: Yeah, it just went over last weekend. We used to go there, and I used to love it, because I just love eating lobster and shit. Every day, lunch and dinner, would be, you know, lobsters and, shit, what was that one place …
Bob: Scallops, and …
Shaun: Scallops and then their chowder is so great, but …
Bob: Oh, yeah.
Shaun: That one Durgin-Park, we’d go there every year …
Bob: Oh, yes, yeah.
Shaun: And the waitresses are all like 90 years old, 80 years old, not that there’s a problem with that, but these old ladies would come up, “What do you want, mister?” It’s like …
Bob: You’re not ready right there, man, you’re not …
Shaun: You weren’t ready, they would …
Bob: You’re not getting served.
Shaun: They’d flick you in your forehead and go, “Hey, let’s go, we got a lot of people here.” I remember, she would bust our balls just on different things, like, “You want the Fred Flintstone,” you know, they, literally, it’s like a Fred Flintstone …
Bob: Prime rib.
Shaun: Prime rib. Big bone, big thing, and, but good times, old, old Boston, man. I kind of miss that. I don’t miss the cold. Shit, I remember every year, it’s always like eight feet of snow when I’m on the roads, and kind of neat, but talk about passionate people out there. I mean, you’d be in a pub at 1:00 in the morning, and they’re singing at the top of their lungs …
Bob: Oh, yeah.
Shaun: At 1:00 or 2:00, remember?
Bob: Yeah.
Shaun: We’re like, we’ve got to be at the booth at 8:00 the next day, and we’re like, “Oh, no.”
Bob: The Celtics fans, the Red Sox fans, the Patriots fans, the Bruins fans, I mean, they’re all so passionate about their teams.
Shaun: They really are, and I remember just recently, back in ’08, 9, with the Lakers, because we’re big Laker guys, and the Boston Celtics, and I remember just the fans, the Lakers are leaving after the third quarter, or whatever, just because it’s, they’re down by 10, and these Boston fans stick with you …
Bob: Heckling, yeah.
Shaun: And they’re in your ear, they’re the biggest hecklers. I freaking love that. I mean, they just get into it, where we’re all, not we, I mean, I get into it, but a lot of our fans are just, “I want to go home and sit in front of my 80 inch TV,” and they’ve just got so many options, where those, I remember one year, we were up like 20-some odd points, and then this guy kept yah-yahing the back of our heads, and I was with our two sons and my wife, and I remember Kyle, our oldest son, was, kept going, “Dad, I’m gonna punch this guy if he keeps going on.” I go, “Just let it relax, we’re winning,” and then the freaking Celtics came and beat us at the end.
Bob: Oh, jeez.
Shaun: Here’s my 20 year old son, ready to throw down with these Boston guys, and he just kept yapping, like a crow, like “rapbraprapraprap.” We got great seats and this guy, he couldn’t do nothing, but you know, I kind of shook his hand afterwards, like, “Dude, you stuck with these guys. You kept after it. Good for you.” Kind of, you know, I wish our fans had more passion like that. I know there are some fans, but anyways. Okay, let’s get that on, let’s talk a little dental. Bob, you get a gazillion calls every day, you see a gazillion cases every day.
You’ve been with me from day one here, but I just know with implants, it’s one of our fastest growing areas in our laboratory, and we have more and more of the GPs, the general practitioners, doing implants. Sometimes, you know, these guys will take a weekend course, you know, and they’ll learn how to pull a flap back and sink an implant in your head, and they’ve got big balls, and they come back on Monday and they start doing it, and sometimes it’s, you know, it’s tough.
Bob: Sometimes, you’ve got to call timeout on these, and you’ve got to get back to basics. If you want a predictable result, you’ve got to use good systems. You have to have your systems in place for success. A weekend course, you can learn a lot, but unless you have good support from your manufacturer, still maintain the relationships with your surgeons, with your periodontist and with your oral surgeons, because not every case is going to be perfectly straightforward. I would say that at least 50% of the cases, GPs are more than qualified to put in the implants, you know, but have good systems in place for planting, know the anatomy that’s in the area, know what to look for ahead of time.
I would say the biggest issue is, try to have a restorative plan in place before you select the fixture, because there are some systems that will offer you all options, but there are other systems, there are other manufacturers and other implant styles that lock you out of certain restorative plans.
Shaun: Kind of like an open architecture of a, they shut it out where you have to use it. What you’re saying is some guys will just go to the top drawer with what they have in there, and they’ll put it in there sometimes, and that’s …
Bob: Then you’re keeping your fingers crossed, hoping for a great result. There are a number of great manufacturers available, and there’s more and more coming into the U.S. every year. It does, it keeps the cost down, but luckily, the more popular brands are, again, they’re becoming more cost effective. They’re becoming more cost effective for us as a laboratory, but also for you guys as the, either the surgeon or the restorative doctor. We have a number of manufacturer specific milling systems we can go with. We can go with Nobel, we can go with Straumann, we can go with 3i.
Those are three very popular manufacturer specific milling centers that we utilize on a daily basis here at Keating, and you know, for a lot of other systems, we’re able to utilize Atlantis components, which is, you know, it was, been taken over by Astra, and now it’s Dentsply, so they have a lot of options for you as well.
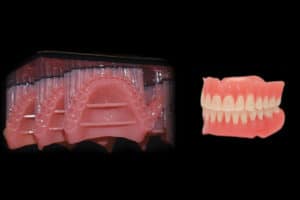
Some of our more popular restorative methods to help keep the cost down, and I’m talking in the high twos to low threes, so it’s still, it’s a very cost effective restoration, is the screw-retained BruxZir, our screw-retained KDZ BruxZir, and our screw-retained KDZ Bruxer® Aesthetic, those are selling from the high twos to the mid threes, and you get a manufacturer specific, what’s called a titanium base, some vendors call it a universal base, where then we can design the BruxZir crown on top of it, and we’ll lute it here in the laboratory for you.
If there are pathage rot issues with proximal contacts, sometimes it’s best to let you guys put in the base, put in the crown, adjust the contacts, and then you can take the universal base out of the patient’s mouth, put it back on the model, and you can cement it extra-orally, so there’s never the issue of cement sepsis.
Shaun: What about with a titanium base? Sometimes the doctor will want like a zirconia base. Is that just, is it asking for trouble, or …
Bob: You could do it.
Shaun: Are we loading and loading on that, or …?
Bob: I think our preference here, you know, the cases that we see back for fracture and …
Shaun: Are not many.
Bob: I think, but, are not many, but you want a titanium to titanium connection, because when you torque the screw down, you want to make sure that you have metal around the screw head for protection. The ones that we do see back that, you know, these have been in the mouth, you know, three, five, seven years, a long time, they’re the ones, unfortunately, where you have a zirconia to titanium interface, and those are the ones that, unfortunately, we see back again. It’s not many, but it is sometimes a bigger issue, and it’s a pretty big inconvenience for your patient, and obviously for the doctor, to take that out and to restore it in a more conventional method.
Shaun: What’s the deal with, remember going to natural dentition with implants, you’re not supposed to tie to that natural dentition, supposedly, because of the movement, and, is that still …?
Bob: You know, the last I heard, when I was at the Kois Center a couple years ago, that the research is inconclusive on that, and it’s more of a practitioner feel, if you will. We do, we do restore a large number of cases where we’re actually connecting an implant based restoration to a natural tooth, in, you know, a three-unit bridge, okay, so the person lost, the patient lost tooth number 19, then they lost number 18, well, the surgeon goes ahead and puts an implant in the position of number 18, and you construct a three-unit bridge from 18 to 20. It’s a very, very predictable solution.
Shaun: That’s, I think I got that.
Bob: Yeah, I think so.
Shaun: That Straumann we did all right.
Bob: Right, right.
Shaun: Well, back in my day, it’s, we couldn’t restore a tooth, with, you know, a single mom with six kids, it’s called extractions. You extract it for $10.00 or whatev- I don’t even know the cost back then, but yeah, then, so we put an implant bridge there, that Straumann. Straumann’s a pretty big time, pretty, kind of one of the more expensive for the dentist. Is it kind of higher up, like …?
Bob: Well, they are, but …
Shaun: Are they coming around in their pricing for GPs?
Bob: They are, absolutely. Yeah. The restorative components, you know, for us, used to be very high. They are coming down. The Straumann milling center, it’s in Arlington, Texas, we get some great products from them.
Shaun: Really?
Bob: Yeah, we’re getting phenomenal custom abutments, we’re getting the, it’s called a variabase, so that universal base or that tie base I was talking about earlier, we get great parts from them for that.
Shaun: That’s, like, open architecture you use with other products?
Bob: You can, yeah, so if you had a …
Shaun: Not that you’d want to. I mean, it’s kind of like a doctor with his impression material, “Okay, I got this body from Kerr, and then I got this watch from 3M,” and why mix and match? “Well, I got this for 50 cents cheap-” I mean, some dentists, it’s like, don’t mix and match.
Bob: Right.
Shaun: If you’re going to use a system, use what they recommend, what their R&D went through and all that, instead of trying to be your little MacGyver of saving time and/or money, when you’re kind of going to lose your butt …
Bob: At the end of the day, at the end of the day, I honestly believe you’re going to get a more precise fit if you’re using manufacturer specific parts. We do, there are a lot of, I hate to use the word knockoff, but there’s a lot of more cost effective brands on the market that are sort of copies of some of these more tried systems that have been in place for a number of years. You can often get good results with that. I’m not saying to …
Shaun: It’s more like screws. Isn’t there separate screws you can use that aren’t the $80 screw, where you can get them for 20, or you know, just different …
Bob: Yeah, absolutely.
Shaun: Things like that, but then again, torquing and regulations on how is that benISO 9000 spec-ed, and is it FDA approved, type thing, that don’t …
Bob: Those are available, yeah, and the FDA is a big issue in our industry, on the implant side, definitely. That’s why we really made the switch, probably three years ago, to maintain the manufacturer specific parts.
Shaun: Yeah, that’s good, because we were getting told, “Just use this and use this,” when we shouldn’t, really, we got to just say, “Hey, we got to do it by the book, okay?” Especially when we guarantee everything, you know?
Bob: Right.
Shaun: We don’t charge for remakes, and so, when we start a case, it’s, we marry that case, so …
Bob: Absolutely. You know, the warranty, with us, is huge, and we’re going to back that up every day, and if there’s an issue, we’re going to help, we’re going to help you, the doctor, and we’re going to be there for your patient at the end of the day.
Shaun: What about when you, it seems like we get a lot of calls, when they’re taking the impression, like, is it open tray, is it closed tray? Why do we get doctors, and some of these guys are big time guru type guys, and they just, they cut a corner here and there, and it’s like, “Dude, no, please.”
Bob: I would say the first thing is, no triple trays. That’s going to distort the vertical relationship on their end. We do see some triple trays, and unless you’re taking …
Shaun: What about if the triple tray’s taken just for the impression itself, and then, you know, you’ve got the opposing, but you take a separate opposing on a bite now?
Bob: You can, well, you can take …
Shaun: You’re still, the tray’s kind of rigid, or it’s not rigid, or …?
Bob: Yeah, so, if you have the healing cap on, and you want to take a triple tray for the opposing, and give us an idea of the adjacent dentition on the working side, yeah, that’s fine, absolutely no problem with that, but once you uncover the fixture and put in the impression post or impression coping, I would say no, no triple trays at that stage.
Shaun: Okay.
Bob: If the patient’s already come back from the surgeon, or if you already have the abutment in place, and you’re treating it like a natural tooth, almost like a natural tooth abutment, where you isolate the margin, you know, pack cord, or trim it with the laser, fine. Again, triple tray generally will work out okay, but if you’re at the fixture level, and you’re using a metal impression, coping, or post, no triple trays. We’ve unfortunately learned that, pouring these models up, the vertical relationship, it’s going to look fine on the model.
Everything always looks fine on the model, but when you transfer it to the mouth, oftentimes, the vertical relationship is disturbed, and the margin height of the abutment that we construct for you is going to be off, the proximal contacts are going to be off, and the occlusion’s going to be off. I recommend, if it’s single units, or two single units adjacent that are not going to be connected, closed tray is fine.
Shaun: Okay.
Bob: No problem there. Some of the general rules on closed tray are, use as much heavy body, or high viscosity material as possible, because you’re not capturing margins. Use it on the proximal contact surface, use it on to occlusal of the adjacent teeth.
Shaun: What material do you like for impressions for smaller stuff? I mean, which are, you know I’m an Impregum guy. What’s yours?
Bob: You know what? Again, Impregum gives us the most accurate, you know, the 3M imprint material is also very good.
Shaun: Is it Imprint II now, or is it …?
Bob: I think it’s, yeah. I think it’s Imprint II.
Shaun: It’s their polyvinyl.
Bob: Correct.
Shaun: Damn, 3M, man, I just, it’s a little more expensive, but at the end of the day, when it comes to consistency and getting that accuracy, why cut corners?
Bob: Right.
Shaun: A lot of guys do.
Bob: Yeah.
Shaun: I mean, I think we always did, back in the day, if we didn’t have the money. Same thing with clothes. You’ve got to buy from Zody’s or, you know, or Kmart. You can’t go to Nordstrom’s and get your good shirts, you know, until you get older, wiser, and more money.
Bob: You’ve learned from a couple mistakes along the way.
Shaun: You learn that those shitty shirts last about three months, and, where the other ones last a year.
Bob: All the buttons are falling off. Yeah.
Shaun: What about with, on your open tray, explain exactly an open tray and closed tray, and the different, and …
Bob: With an open tray impression, you’ve got to, you know, you or we will drill holes on the occlusal table, perforate the tray for you, so the pin will be exposed. That open tray impression coping stays within the impression throughout the entirety of the period. It’s in, the impression coping is in the impression in your patient’s mouth, it’s in the impression while it’s in transit to us, and it’s in the impression while we’re fabricating your implant cast. There’s literally, there should be no variation. There should be no distortion, and it should be 100% accurate. We know that not to be 100% true, but that’s in theory.
Closed tray, however, is you put the impression coping in, seat the tray with the material, let that set. After it’s fully set, you remove it, and the impression coping will stay attached to the fixture in your patient’s mouth. You’ll unscrew it, put it in a little sterilization bag, you know, indicate, an indicator line, you know, even a Sharpie pen, for us, is great, just which side is buckle, just something simple like that. A lot of doctors will take a bur and score the buckle side for us.
Shaun: Yep.
Bob: Yeah. That way, it just gives us another landmark to line up, because we’re going to have to attach a laboratory analog to your impression coping, reinsert it back into your impression, and then fabricate the cast. Again, there are two potential sources of air, and that’s, you know, that one is in the office, and one is here in the laboratory.
Luckily, most impression copings, closed tray impression copings, have sufficient vertical height, and have sufficient retentive surfaces, that, you know, we’re using loops and we’re using a scope when we’re assembling them out on the lab floor prior to going into the model room, and we’re obviously, we’re being as careful as we can. Most good brands of implant impression copings, we’re able to tell, we’re able to orient, no problem.
Some of the other ones, where you have insufficient vertical height, or they’re mostly cylindrical, or they only have maybe one retentive surface for us to align into your impression, those can be a little tricky, so if you’re visually inspecting your impression coping and you know, “Oh, it’s, this is just, it’s like a pencil, and I don’t know which way it’s going to go back in,” just kind of think about what we have to go through at the next step to make your cast accurate.
If you just give us a head’s up, “Hey, I drew a black Sharpie line on the buckle,” that way, Steve, Manny or I, when we get it here in the laboratory the next day, we’ll know how to align it properly. Again, more information for us is always better. You know, we get lab slips with nothing on them. It’ll say tooth number 30-A2. You know, just give us a little bit of something to go by.
Shaun: Yeah, exactly. I mean, usually, it’s anteriors, and you know, they have nothing, no study model …
Bob: Right.
Shaun: And it’s just like, A3, and it’s like, “Well, dude, where’s my,” you know, “Where’s my study model? We’re just going to make it beautiful natural, but more information is better.” Now, when you were saying on those trays, closed and open tray, is there trays already built and made that way that they can buy, that’s already set up and ready to go?
Bob: Yeah, we actually get a lot of stock plastic trays with very tall side walls, and you just take a round burr, take an acrylic bur, just punch through where the pin is going to stick up through, and yeah, those work fine.
Shaun: There’s not, none that are pre-made, that you can buy them that way, no?
Bob: No, I’ve …
Shaun: I guess there’s not a big use for it, probably, or …?
Bob: I haven’t, you know, I haven’t seen, I haven’t seen one that’ll come with the holes pre-drilled for you. It’s easy enough to do, and we do them here. We make custom trays for your customers every day.
Shaun: Yeah.
Bob: We’ll pre-drill the holes for you, but that requires a preoperative cast and you know, at least where the healing caps are in place.
Shaun: What about with, I hear, when I have issues, when they usually get to me at my desk, it’s a lot of times is the collar height, and I know with a, digitally, we just have space, and now, I think we have it to where we can digitally put in a tissue area there, but more and more I hear it, when a doctor’s not telling you, “Okay, let’s go supra,” you know, a half millimeter supra, from the tissue, or, “Let’s go sub, a millimeter, two millimeters,” but we’ve kind of got a hard tissue on a stone model.
We do soft tissue models, but a lot of times, you know, when a patient’s an upper, you’re not usually lifting your lips up to show your single, you know, your gingival third. Lot of, 90, I don’t know how many …
Bob: Right.
Shaun: Lot of people don’t show that, but yet, and that’s where a lot of guys in conventional fix will keep it just at the tissue, okay? Even a little supra. A lot of old guys, you know, the strups and everything else were the feldspathics, remember? Everything was supra, and it’s just right there in the enamel, and that’s just, you’re never going to see, but some people have, like my wife, she smiles and you get gums and you get all smile.
Me, lot of guys, you don’t see, and especially lowers, you’re not going to be able to pull your lowers back, but more and more, I’m getting, you know, the thing was 4 millimeters below the tissue, and it’s like, you know, I don’t like, you know, you’ve got your attachment down there, and tissue, and everything else, and just, everyone always says, you know, a lot of guys say, when it comes to setting your margin, when we’re doing PFMs, I like going sub myself, and bury it in there, but it’d be nice to have a nice sloping chamfer or shoulder.
You don’t want to have some shoulder bevel, because then I’m coming with metal, I’m coming with opaque, I’m coming with porcelain, and by the time you get done with that tissue, you’re blanching that tissue.
Bob: Right.
Shaun: It’s just, the burden profile is too thick, on and on. Well, on the other way, what’s the best way to really know … Like you said, we have to, Dr. [inaudible 00:29:17] index, where it’s at, this in there to help us there, but what about when it comes to tissue, because, should everything be a soft tissue, totally, or when it’s coming to, you know, a digital type model, where the last few I’ve seen, they have a little insert now …
Bob: Yeah. I know.
Shaun: That’s kind of bitching, but then again, that’s a guesstimation too, because that’s hard, and then, if you’re going a little bit sub, I mean, where, where does that collar go? Where should it go, and do you see problems with that coming in to us?
Bob: Absolutely, yeah. I mean, cement sepsis, cement contamination, and loss of bone around the fixtures, it’s pretty well-documented that cement left in the salkus on cement retained restorations is a big problem.
Shaun: Yeah.
Bob: More of your customers are going screw retained. The screw-retained BruxZir that we talked about, screw-retained Emax, screw-retained PFM, are all very predictable solutions to overcome this problem. We do, even this day, we do an awful lot of casts, UCLA based restorations for single unit crowns.
Shaun: That’s because we want to bring it where we want it, or no?
Bob: Well, yeah, we can control margin depth, but we’re also making it essentially, it’s a one piece design, it’s no cement. There’s no cement anywhere in it. We’re casting …
Shaun: That’s where we’re cementing it ourself here, or …?
Bob: No, we’re casting a UCLA gold and plastic abutment for a crown. We’re waxing up, your waxers are waxing up and giving the ceramist the proper support, and then the ceramist is applying porcelain directly to the metal, so there’s no cement. There’s never any cement that’s going to come in contact with the patient. It’s a PFM restoration.
Shaun: Okay.
Bob: Those sell for the high fours to the mid fives, you know, because it’s an expensive part from the manufacturer, and it consumes that …
Shaun: Something, is that like a Atlantis type abutment, or no?
Bob: We can do that with Atlantis, also, but we will then construct a PFM coping and your ceramist will apply porcelain to that, and then after it’s been final QC, your two implant waxers, one of the two, will lute the two pieces together. It’s a screw retained PFM on an Atlantis abutment.
Shaun: Have we, do we get many of the interfaces that we’re luting together come apart, or no?
Bob: No. We’re trying to avoid that whenever possible.
Shaun: What are we luting with?
Bob: We use Ivoclar’s multi-link implant, so that’s one of the best that’s on the market. It’s a very trusted brand here in the United States. Ivoclar is really the pioneer when it comes to all ceramic materials in this country.
Shaun: They are the bomb.
Bob: Yeah.
Shaun: Well, good job. What else, for a doctor doing implants, starting off, what other recommendations, not even just using our lab, but what could you give, because that’s what we’re here doing. We’re trying to give advice to doctors to help them practice better dentistry, easier dentistry, more predictable dentistry. What else can you throw at them for implants, what you should, what you shouldn’t do, what you should get, what you shouldn’t get?
Bob: It’s really, it’s planning and communication, that’s number one and number two, is, you know, we get a lot of cases, and we hear a lot of times on the phone where the patient has returned from the surgeon and now I’ve got to restore it, and now what do I do?
Those are hard things to manage, because really, the fixture’s already been placed, and if it’s at an off angle, or if it’s too deep, or if it’s super gingival, you’ve got a lot of obstacles that you have to overcome at the restoration level, at the abutment or the restoration level, and sometimes you cannot undo these problems with surgery, and I would say that, you know, more planning the better. It kind of goes back to what, with surgeons in hospitals and even carpenters, you know, you measure twice and you cut once.
Shaun: Yeah.
Bob: The more you can plan, the better off you’ll be in the final restoration. Number two is understanding some of the design limitations, understanding some of the limitations that your patient already has, and you’re going to ask the restoration. The biggest one we get is closing gingival embrasures. Well, a lot of times, when you’ve got any dental space, and you’ve got the two teeth adjacent to it, well, they’re going to tip, and they’re going to close the space a little, well, that creates an anatomic undercut on both sides of the restoration we’re going to make. It’s not an undercut in our restoration, it’s an undercut in the adjacent teeth.
Shaun: Yeah.
Bob: Some of our high volume implant customers are advising their patients, “Hey, I’m going to need to add a little composite. I might need to do an MO and a DO adjacent. I might need to fill in this space, or if the space is closed too much, I’m going to need to do a little bit of enameloplasty and smooth out your adjacent teeth so that the laboratory can then create a restoration with a longer, broader contact area to help prevent the food from packing in there.”
These are just some little things to watch for, because I’ve unfortunately heard it from my father, who has to restore the implants, and you know, “Oh, Mr. Jones is back and he’s complaining of packing food on the mesial surface of number 30. It was an implant crown you guys did three years ago.” “Okay, Dad. Well, you know what? Hey, this is our crown and this is the distal surface of number 29. See that anatomic undercut? We can eliminate that and you can help Mr. Jones out here, but it’s going to require a modification on the restoration that’s on the tooth in front of it.”
If a little bit of communication with the patient can make you a crown, the laboratory can make a great crown, but in order to help prevent food impacting there and to close this gingival embrasure space properly, we’re going to need another restoration, or we’re going to need a modification of the restoration that’s already on the tooth in front of it.
Shaun: Isn’t there some sculpting of the tissue? I know, you’ve got an implant here, and then you’ve got this big space, and we can only come out from the margin here, and then you’ve got to go over …
Bob: Yeah.
Shaun: It’s hard, but if we trough that tissue there, we can jet out there, but a doctor doesn’t really go in and …
Bob: You know, in the anterior, utilizing custom healing caps to really get the tissue where you want it to be, you’re setting up an ideal emergence profile in the abutment and restoration that we’re going to make next. It takes a couple months.
Shaun: Yeah, it really does.
Bob: It’s really worth it, particularly if you have a single anterior tooth …
Shaun: With a high smile line that you’re seeing?
Bob: Yeah. Yeah.
Shaun: That’s our biggest thing is, we call them black triangles, and it’s in your mouth, and when you’ve got a high smile line, and you look through, and you don’t have your embrasures closed all the way, they’re black triangles. They look, there’s that space, but it just looks like, it just looks terrible on your teeth when you’re looking through. It just looks like black holes, kind of, and it just doesn’t look natural.
A lot of times, the doctor will say, “When your spit or your saliva fills in a lot of naturally triangles that you had,” you can kind of fill it in when you’re doing pictures, but other than that, it’s just gingival recession, a lot of it, and you’ve got those black triangles, and that’s the dreaded thing, as a ceramist, that I don’t want to see any black triangles, but when it’s coming to implants, and you’ve got these rods here, and we’re trying to close everything up with a nice contour coming out of tissue, it’s hard, because you’ve got to jet it all the way over, and there’s a lot of talent to it.
Bob: Yeah.
Shaun: There’s a lot of talent to it, but a lot of times, too, it’s the dentist not really thinking it out with the oral surgeon or whoever’s placing it, and that’s why, I know, my brother’s an oral, my brother’s an endodontist, so he does his little meetings with his, you know, the GPs and stuff in town. I think it’s good that you keep that relationship and you try to, like if I wasn’t sinking my implants, and I was doing a lot of implants and having an oral surgeon do them, or a periodontist doing them for me, I would probably get on that guy’s good side, especially if you’re not really getting stuff back that you need the way you need it.
Now, wouldn’t it be good for the general dentist to be doing, if that, say that periodontist or oral surgeon isn’t doing panographs and all, well, he’s got to be doing to sink in these implants, but wouldn’t these custom stints be good for us …
Bob: Yeah.
Shaun: And, or guides for the dentist to give to the surgeon, or no?
Bob: Absolutely, yeah. We do a lot of surgical stints where we’re going to wax up the restoration to …
Shaun: Ideally, what …
Bob: Ideally, based on the adjacent teeth, and we’ll make you a stone model, we’ll make you a suck down, we’ll even make a little flipper if you want, for your patient, but you know, having the surgeon understand what the final restoration needs to look like is a huge benefit. Yeah, it’s a little bit more money, but I honestly believe that, if the surgeon has a better idea of what comes next, and if the restorative doctor has a better idea of what the surgeon needs to put the fixture in the correct position, your patient’s going to benefit.
Shaun: Oh, yeah. I’m sure there’s hotshot surgeons out there that really don’t need that little nesbit type flipper in there to show them, because you’ve got your x-ray, you’ve got your pano and you’re looking at it, but I just think a really hot, a great dentist that’s doing these, that wants more consistency and more, you know, to be able to really say where this tooth’s going to be, to kind of give that to that oral surgeon, saying, “Hey, I got Mrs. Jones. We’re doing number 30. Here, we already did the stint and a little nesbit for you to go to put in the mouth.”
You can go off of, you know, correlate it off of your pano, and go ahead and have it to be, you know what? “This is good. Thank you, doctor, for bringing this to me.” He’s going to love that dentist for …
Bob: Absolutely.
Shaun: Giving it and making his job easier, because the times we’re seeing this, this, this, this, with these implants, it’s probably a guy trying to say, “Well, I’ve got freaking bone here only. I’ve got to go kind of,” you know? I just think if you really work with your lab, it does a lot of implants, and then you work with your surgeon, if you’re not doing it, to come up with the best solution to give you the best results, instead of coming in at the end of it all, going, “Well, what are we going to do now to salvage it?”
Bob: Yeah.
Shaun: We do too much salvage work where, think about it at the beginning, try to use the tools that you can to make it predictably accurate, and it might cost 100, $200 more for a little nesbit type partial flipper, and a snap for you, but, a surgical stint, but I think that’s probably the wise way to go.
Bob: Absolutely. It’s much better than having Mr. Jones show up in your office every two weeks complaining about the restoration.
Shaun: Yeah.
Bob: It’s, a little bit more on the front end really does pay off on the back end.
Shaun: Absolutely. I’ve got guys that, “God, I would rather have done three regular crown preps, and, instead of one implant, because I know this is going to go in, they’re going to be fine, and it’s not going to be a headache, where this one implant, I’m seeing this patient for six months,” and it shouldn’t be.
Bob: Yeah.
Shaun: It should be boom, boom, boom, and it does happen. Well, Bob, thank you so much.
Bob: Thank you very … Thank you very much.
Shaun: I really appreciate it. It was short and sweet, but I think, if you guys can get anything out of it, do what you can just to make it more predictable, and I think your implants will go a lot smoother. It’ll go smoother for us, and that’s what we want here. We want to get some good work in here so we can show what we do, instead of just trying to be reactive on stuff that we’re getting. We like to be proactive and just kind of do things right the first way, but I want to thank you all for this week’s, you know, coming and listening to our podcast here at Keating Dental Lab. If you want to get anything on for promos, just go to keatingdentallab.com/promos.
Then, also, for our Dental Up podcast, you can just go to Keating Dental Lab, same thing, slash podcast, and you should be able to pull these up, but again, if you have any ideas or topics you want us to talk about, please let us know. Come on to our Facebook page, Keating Dental Lab’s Facebook page, and like us, whatever that means. You’ve got to, I guess you push on it. Give us a lot of likes. I don’t know why we need them, but I guess we need it for content, but again, I want to thank you all for listening in, and again, thank you very much. Have a great day.