Dr. Hornbrook shows you how to increase your patient’s comfort by effectively using single tooth anesthesia with the STA WAND in Part 2 of the “Practice Enhancer Video Series”!
Learn More about the Wand: thewand.com
What are the advantages?
- *Looks non-threatening and almost cute.
- •Researchers have found that the Wand induces less anxiety than any other injection method (Kudo et al, 2001).
- •The precise control of flow rate and pressure reliably produces a comfortable injection even in potentially more “difficult” areas like the palate, where the tissue is less elastic.
- •Many dentists enjoy the light weight and easy handling. The penlike grasp allows the operator to rotate the handpiece, which can make it easier to glide the needle into the tissue.
- •Two “fancy” injection techniques (the AMSA and P-ASA, for the nerds among you) are much more comfortable and effective when the Wand is used.
Full Video Series Transcript:
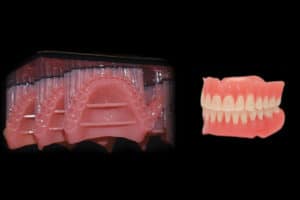
Dr. Hornbrook: Hello. I’m Dr. David Hornbrook, the clinical director here at Keating Dental Lab in Irvine, California. Today I’m gonna talk about what I call one of my practice enhancers. Not only, I think, is it gonna allow me to give more comfortable dentistry, but it also allows me to use technology that I think the patients will talk about when they discuss their dentists in my community. Today we’re gonna talk about the Wand. This came out uh, over a decade ago. It was originally called the Wand, then the Wand 2, then the Compudent, then the STA. Then they renamed it last year the Wand because the familiarity with that name. STA stands for Single Tooth Anesthesia, so let’s look at this. Sh- This is Jake. Jake, do you mind if I don’t wear a mask just for video purposes?
Jake: No.
Dr. Hornbrook: Normally I put a mask on. I promise I don’t have any onions for lunch. All right. So, we’re gonna do a single central on Jake, and the first injection I’m gonna show you is what we call an AMSA, anterior medial superior alveolar. We all know that if we were to introduce 6, 8 or 10 veneers or even a single central, we numb the patient up in the buccal vestibule, and then we try it in, we ask the patient to smile and of course, the lip is like this. Or if we try 6 or 8 or 10 veneers in there, they can’t move their lip, so I don’t want lip anesthetic, I want lip mobility. Also, with multiple units, let’s say I was gonna do 8 or 10 veneers, that’s 8 to 10 different injections sites, and if you’ve ever had an anterior dentistry, or you ask your patients or call them the next night, they’ll say, what was the most uncomfortable was the injection sites. So this is the STA. It has a very small hand piece. I like to use a 30 gauge short. Although it is available in different sizes, this would be a 27 gauge long, which if we were to do an IA, inferior alveolar block, we would use this although in a moment I’ll show you that what we’re doing most of the time, 99 percent of the time, we’re giving PDO injections, not the blocks.
So we’re gonna go ahead and use Septocaine. The way this machine works, it actually is a computer activated anesthetic delivery device, and it works on bla- back pressure. We’ve all given palatal injections where you put the needle in, you squeeze, and it seems like nothing is coming out. All of a sudden, a burst of anesthetic comes out, the patient screams because of the pain and the expansion of the tissue. Then you back up again. I mean … We have a difficulty giving injections especially in the palatal. This anesthetic delivery device can give injections much slower than anyone can do manually, and it measures the back pressure and then delivers the anesthetic to compensate for that back pressure. So we can either aspirate or not aspirate. The nice thing about aspiration is once I take my foot off the foot pedal because it is foot pedal activated, as I pull the needle out of the tissue, the aspiration will actually pull that excess anesthesia that lies in the needle and the delivery wand. It’ll pull that back and suction it back so it doesn’t go in the patient’s mouth.
So we’re gonna go ahead and put the aspirate. We can either leave the STA or not on, that’s the single tooth anesthetic. What that does, it measures back pressure to see if you truly are in the PDL space. Lots of times you know you try to give a PDL, you’re pushing, pushing, pushing, nothing comes out. Other times you push, and it’s just easily comes out of the syringe. You’re probably not in the PDL space. Jake has topical anesthetic in his palate. This where the AMSA injection is. Go ahead and lift your head high. I like to use these optragates from Ivoclar. It’s a non-latex dam and cheek retractor. The best way to put these on is you just wet it, spread it, you can see it has a stiff outer ring, a stiff inner ring. You go ahead and separate the 2. You squeeze in the center. Open for me, Jake. You put one side in, put the other side. Put the inner ring behind the lower lip in front of the teeth and then the upper, and there’s our retraction. You can see we have great retraction. We can utilize this to take impressions because we have our vestibule.
We also, if we were gonna do a calibration especially with horseshoe articulating paper … Tap up and down. You can see he’s able to open and close. All right. Is that pinching at all?
Jake: No.
Dr. Hornbrook: Okay, so chin up for me as much as you can and open as wide as you can. Ideally what we’re going to do, and we’re gonna anesthetize for the single central but even if it was pre-molar to pre-molar, let’s say for 10 veneers, we pick a site, imagine the mid-palatal suture, imagine that line, imagine a line right on the gingival margin of the pre-molars, and then you split the pre-molars. So it’s halfway between the gingival margin, the pre-molars and the mid-palatal suture and splitting the pre-molars so basically right there. Now do you feel that at all? Okay, so the topical has worked. The way we give the anesthetic is we place the bevel of the needle just against the tissue, don’t penetrate through the tissue, against the tissue until we get a little bit of blanching. Then we go and put our foot on the foot pedal, you’ll hear a beep. After 4 beeps, the machine actually comes on and says cruise, which means you can take your foot off the foot pedal. And then we put this bevel after the … After the blanching, we put the bevel just slightly underneath the tissue, wait about 3 or 5 beeps, slightly another millimeter or so, 3 or 4 beeps, another millimeter.
What we’re doing is chasing the anesthetic. Jake, you may feel a little pinch and certainly some pressure, okay …
Jake: Okay.
Dr. Hornbrook: … and it’s probably gonna taste really bad. Open for me. So I’m gonna go ahead and take the bevel and needle, putting it against the tissue on the foot pedal. (Beeping). You can see the tissue start to blanche.
STA: Cruise.
Dr. Hornbrook: There the STA just said cruise. I’m gonna go ahead and put it in the tissue a little bit, 3 to 4, about 4 beeps, a little bit further. Okay. That’s the aspiration, so it’s actually pulling it back into the syringe, the hand piece. All right, so he already has a little bit of anesthetic superficially in-in about the millimeter, 2 millimeters in the tissue, so shouldn’t feel this at all. Do you feel that?
Jake: Mm-hmm (negative).
Dr. Hornbrook: Okay.
STA: Cruise.
Dr. Hornbrook: Okay, 4 beeps. Another millimeter in. Four beeps, another millimeter. Do you feel that at all?
Jake: Mm-hmm (negative).
Dr. Hornbrook: Now we’re gonna go ahead all the way to periosteum. How you doing? Okay?
Jake: Mm-hmm (affirmative).
Dr. Hornbrook: Okay. I’m gonna give him about a half a carpule. Again there’s the aspirate. Let me give him a little bit of water. This is Septo- 4 percent Septocaine, Articaine hydrochloride, and it tastes terrible. All right. I’m gonna do the other side. Turn toward me. Now I’m gonna give an example as if I was, let’s say, seating 8 or 10 veneers, I’d want both sides to be anesthetized. He’ll have anesthetic, full tooth anesthetic and the palate from the first molar to the first molar and about 10 percent of the time, I get some buckle anesthetic but no lip anesthetic, so same thing. Right against the tissue.
STA: Cruise.
Dr. Hornbrook: One, 2, 3, 4, go about a millimeter in, 2, 3, 4, okay, let me give you a little bit more water. Now I’m gonna show you how we do the PDL injection. Close and swish a little bit if you can. Now as I mentioned earlier, rarely do I give inferior alveolar blocks even for lower molars, and I do a lot of dentistry, so it’s not that I’m just doing anterior forward. So on the first molar, open real big.
Again, I like to use the 30 gauge short. I bend it a little bit. Turn toward me. I’m gonna do the first molar, mandibular right first molar. You can put a little bit of topical or not. Usually you don’t feel this. You’re gonna feel a little pinch though. I put it down into the space firmly, put my foot on the foot pedal.
STA: Cruise.
Dr. Hornbrook: Watching the STA device to make sure I truly am in the PDL space. Oh, usually give about 10 beeps pushing firmly into the space. Then that’s the aspiration. I’m gonna give you a little bit of water. Close and swish. Did you feel that much?
Jake: Mm-hmm (negative).
Dr. Hornbrook: Now typically what I’ll do is I’ll give it in 4 locations. Open real big. For molars, I’ll go at the distal lingual line angle, the mesial lingual line angle. Sometimes that’ll do it, but I like to ensure that my patient is numb. I will go the distal facial line angle and the mesial facial line angle just into the PDL space. Again, you’re pushing hard basically until you’re hit bone, and you’re in the space and typically I’ll give about a quarter of a carpule, maybe a half carpule uh, for a hot tooth. That’s the total anesthetic I’ll give for that single tooth. The advantage of that is he will be able to operate his tongue. His lip will not have anesthetic, he’ll be able to function normally. All right. So again, those are just 2 injections. We can give mentals. My hygienist actually use it especially when he does scaling and root planing because, again, less anesthetic, more comfort. It’s not the syringe that’s coming at the patient. That certainly elicits anxiety with many of our patients.
And the benefits as I look at this instrument, one is less patient anxiety, which is huge for me. Second is less anesthetic, which I think we should always to try to avoid using excess anesthetic. Third is that the patient is much more comfortable after the procedure. You know, I always say that if I did a DO filling on, on um, Jake, after I polish and adjust occlusion, he leaves, I’m done with Jake. He’s not done with me, he’s still numb for the next 45 minutes to an hour especially if I give an inferior alveolar. With this type of injection, he’s basically numb, very limited residual effect on the anesthetic. And fourth, as I mentioned earlier, just the marketability when he goes back to his office, and he said he just want to the dentist, and they say, oh, how come your lip’s not dripping. Well, and I say, what that is the type of anesthetic and the type of injection using the STA. So I hope that helped in uh, certainly educating a little bit about, again, one of the quote, unquote I call my “practice” enhancers, something I use in my practice every day, and I can’t imagine working without it. Visit us for other videos and some of the very cool education we’re doing here at Keating Dental Lab.