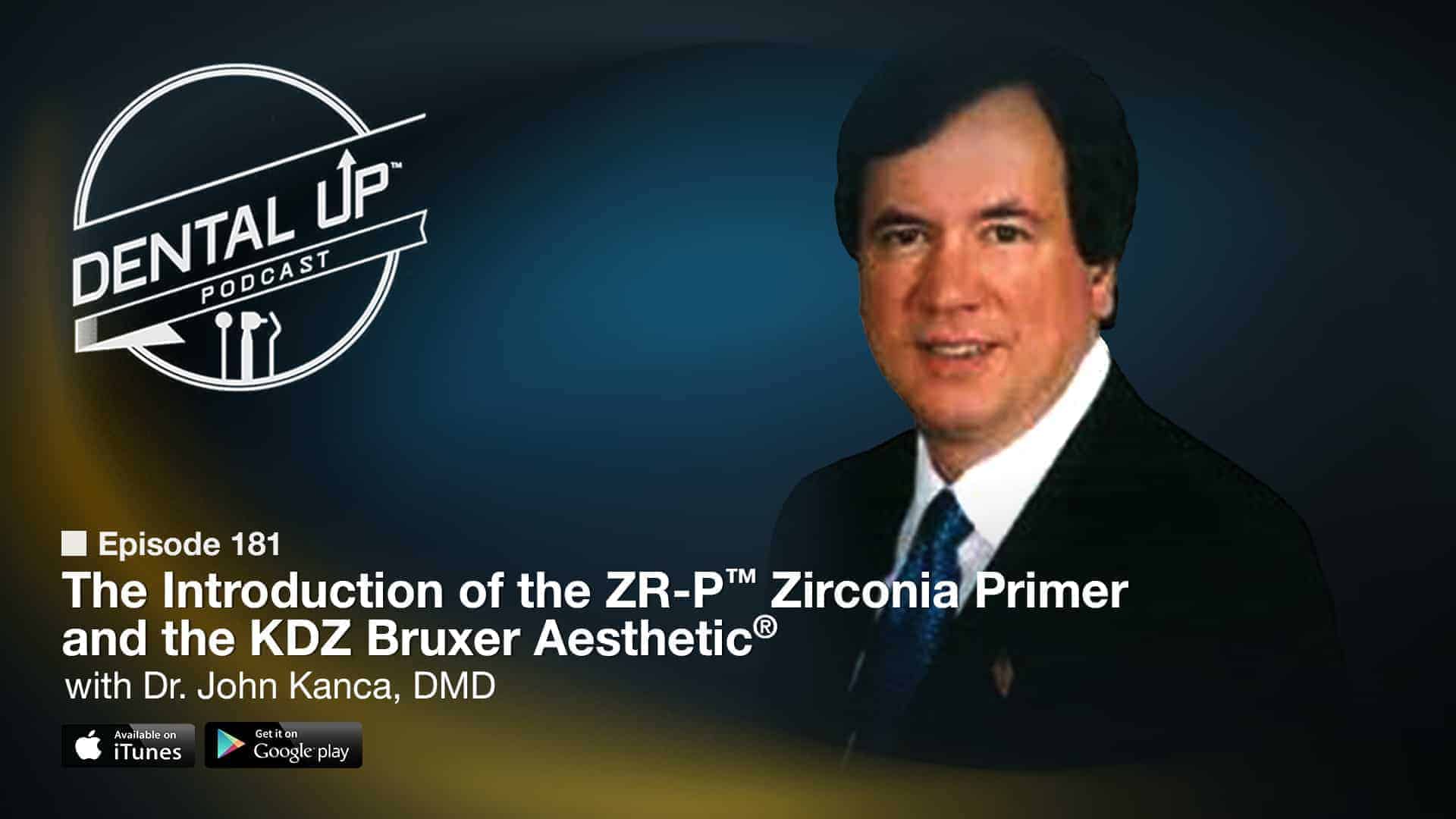
Our Dental-Up Podcast guest this week is Dr. John Kanca, joining our guest host Bob Brandon as they discuss Dr. Kanca’s process in creating the latest product addition to Apex Dental Materials, ZR-P Primer. Dr. Kanca explains the testing process and the positive results when prescribing the KDZ Bruxer® and KDZ Bruxer Aesthetic®. He explains why it’s important to use a high quality light source when working with zirconia materials. You will also learn Dr. Kanca’s clinical protocol for cementation with the Apex Dental Materials line-up, including PFMs and lithium discilicate, and PFM restorations. You will hear all this and more on this week’s episode of the Dental Up Podcast.
In this Episode you will hear about:
-Dr.Kanca explains his rationale for prescribing KDZ Bruxer Aesthetic
-Dr. Kanca’s testing process of ZR-P on the KDZ Bruxer
– Why having 2mm occlusal reduction in the central fossa helps the lab create functional anatomy without complications.
– Dr. Kanca’s clinical protocol for cementation using the Apex Dental Material line of products on zirconia, PFM, and lithium discilicate restorations.
-The Importance of utilizing a high quality light source when working with zirconia materials.
For more information on Dr. Kanca’s practice or for more information on The Apex Dental Materials, check the links down below.
Practice Website: http://middleburysmiles.com
[bg_collapse view=”link” expand_text=”View Full Transcript” collapse_text=”Hide Transcript” ] Host: Ladies and gentlemen, this is the Dental-Up Podcast brought to you by Keating Dental Lab, a full service award-winning dental laboratory. Each week, you’ll learn tips and techniques from real world dentists, bringing you in depth interviews, motivating stories, current events, and sports. Here’s your special host, Bob Brandon. Bob Brandon: Welcome to the Dental-Up Podcast. I’m Bob Brandon, general manager here at Keating Dental Lab, filling in for Shaun today. I’d like you to welcome one of the truly brilliant minds in dentistry. I’ve been influenced by a lot of dentists in my technician career, but two more so than any others. Both have the initials J-K. The first is Doctor John [inaudible 00:00:50] and the second is our guest today, Doctor John Kanca. I first met Doctor Kanca in 2004 at a hotel lobby during the Yankee Dental Convention. Shaun and I were sitting there at the bar and in walks Doctor Kanca and his crew. We say to each other, “Oh my god. That’s John Kanca.” Acting like we were in high school, “You go talk to him,” “No, you go talk to him.” Finally, we did. After several more drinks, he started to send us cases to the lab. Doctor Kanca is one of the founding members of the AECD. He’s also the past president, the fourth president to be exact. Digest that for a moment. One of the founders and the fourth president of the AECD. He’s also the recipient of numerous awards, too many really to list here. Bob Brandon: He was awarded the Gordon Christensen Lecture Award in 1995 at the Chicago Mid Winter Dental Society meeting. He’s also a consultant to numerous dental materials companies and he founded Apex Dental Materials along with Scott Lamerand and Chris Colton. He’s been in private practice in Middlebury, Connecticut since the early 1980s. He’s a true pioneer in adhesive dentistry creating solutions for practicing dentists around the world. If you ever have the chance to listen to Doctor Kanca speak live in an event, do not miss it. I guarantee you will learn more from his lecture than any other CE course out there. He lectured on etching dentin at the AECD in 1989 and was ridiculed, but less than three years later, his ideas were transformed into Kanca Bond or the Kanca Technique. Most of us know it today as Bisco’s product All-Bond. Please, help me welcome my guest today all the way from Middlebury, Connecticut, Doctor John Kanca. How are you, Doctor Kanca? Dr. John Kanca: I’m well, Bob. How are you? Bob Brandon: Excellent. Thank you. I want to thank you for joining us. I know you’re tremendously busy and involved in so many different areas, but thank you so much for taking the time out of your schedule to spend the next half hour with us. I know you’ve been our guest several times, but what I’d like to focus on today is some of the newer products from Apex Dental Materials and some of the reasons why you, Scott, and Chris decided to create the newer products, particularly the ZRP, the zirconia primer. Dr. John Kanca: We’re always interested in advancing dentistry and creating things that are particularly useful. The philosophy, to be honest with you, in Apex, is to obviously make things better, but we create things that I need because I am just your average general dentist. Bob Brandon: You’re not average. Dr. John Kanca: When I have a need for something, when I see something missing that I’d like to have that I try to instigate the creation of such a product and pursue that. That’s where we come from. I know if I need something, I can call him and say, “Look, this is what I’d like to have and I’d like you to make it for me. Let’s do this.” That’s how the progression goes. Bob Brandon: I can attest tot that first hand. My own father, he started off with simplicity and then went to Interface, Surpass, and finally Clean & Boost. Your products have, although I know you don’t know him, helped him in clinical practice for the past 15 years. It’s been phenomenal. I don’t think he goes a single day without using one of your products. Dr. John Kanca: That’s always great to hear. I always appreciate that kind of feedback. Bob Brandon: Tell us a little bit about ZRP, your zirconia primer, and how you’re using it in practice because I know, but our listening audience doesn’t know you’re utilizing a lot of our KDZ Bruxer aesthetic, our high translucent zirconia. Walk us through your procedures from when you seat the patient down in the chair, how you take the provisional off, how you prepare or re prepare the preparation, then try in the restoration, and then to final cementation if you will. Dr. John Kanca: Not every zirconia crown is bonded, but we have not with the advent of the zirconia primer, I started now to pursue some partial coverages and onlays. I think that’s where this really tends to lend itself very nicely or short clinical crowns. In those cases, you want to be bonding something on because you’re concerned about retention. It took a while to crack the code on producing the primer, but I finally did it. We’ve tested this now. We’ve done some long term storage on it, medium bond strengths, and then store it long term. The material is particularly stable. As you know, I took great pains to make sure that the samples I was testing, that I was utilizing, were exactly the same as was being produced and sent out by Keating. Actually, we took some crowns that I guess were going to be disposed of and we used those in our test because I had gone through several sets of materials that the materials seemed to work really well, but I wasn’t convinced it was exactly the same as what we were seeing in the office, the kind of materials exactly that we were delivering, so I took great pains to make sure that was exactly the case. Dr. John Kanca: Once we did that, we got these wonderful numbers that we’re getting, only then did I feel confident to say, “Yes, we have this and we have it nailed.” As far as how we used it, if it’s a crown, we typically will cut the preparation and seal the preparation with an adhesive, usually Surpass. We could do it with Superb as well, but usually it’s with Surpass. We’ll seal up the preparation the day it’s cut. We have already made the temporary. Then, we’ll wipe off the oxygen inhibited layer with some alcohol after the adhesive is light activated. Once you place the Surpass, you have to make sure you thin it out as much as you possibly can. Then, you light activate all the surfaces. Then, we wipe off the oxygen inhibited layer. Then, seat the temporary with anything you want. It could be Temp-Bond, Temp-Bond NE, or if you need the extra retention, there’s UltraTemp from Ultradent. Then, the patient goes home. This would also be true of partial coverages. Dr. John Kanca: When the patient returns, we’ll remove the temporary, we’ll clean off the surface trying not to disturb too much the adhesive that’s in place already. We’ll use [inaudible 00:07:59] to remove some of the old temporary cement, scrape off the rest, clean it up, and if we feel it’s appropriate or we need to, we’ll reapply Surpass Two maybe or Surpass Three just to freshen in up, or Superb again if that was used just to freshen it up a little bit. Thin it out. That again is necessary and thin it out as much as possible. Light activate that. Then, the ceramic crown or onlay, the zirconia or modified zirconia, the KDZ Bruxer, or Bruxer aesthetic, whatever we have, we’ll take that typically … Now, what we would recommend if you’re not going to … You can either sand blast the inside, if you don’t want to do that, then what we would recommend is you clean the inside with sodium hypochlorite, rinse it, and dry it. Then, apply the primer, just put a coat of the primer on, thin it out as much as you can, then apply a coat of Surpass Two or Superb. Thin it out as much as you can and light activate it. Dr. John Kanca: Then, you can cement it with, for the most part, either Anchor. If you’re really quick, you could use Injectafil. To be candid, you could also just go ahead and cement them again with a Resin-Modified Glass Ionomer because this will add greatly to the retention of an Resin-Modified Glass Ionomer. You have actually a number of choices as to the looting medium. Treatment of the prepared tooth and the zirconia prosthesis are pretty much the same no matter what you do. Bob Brandon: Did you observe any differences in bond strength or degradation over time between our two different types of zirconia, the high strength Bruxer or the high translucent Bruxer aesthetic? Dr. John Kanca: I have not. The reason I have not is I haven’t been sent any of the rejected the Bruxer aesthetic crowns. Bob Brandon: I can get those to you. Dr. John Kanca: If I can get my hands on some of those, I’d be more than happy to test that for longevity. Bob Brandon: The material composition is nearly identical. Dr. John Kanca: Yes, I know. It’s just the centering. I think that we would see very much the same thing, but I would be happy. Again, I won’t tell you I know, but I’d like to test it. Bob Brandon: Yes, absolutely. You brought up an important point earlier when you were describing the painstaking process of being absolutely sure. I didn’t fully appreciate that you wanted the crowns to be in the absolute final state before we shipped them to a customer. That’s what you needed to test. We were so concerned with getting the shape right, the thickness right, and the centering right that I failed to recognize that you needed to test what every clinician in the country and around the world was going to be delivering. I will get the Bruxer aesthetic samples out to you by the end of this week for sure. Dr. John Kanca: That would be great. To me, you need to replicate the clinical conditions as closely as you can. Before I could tell anybody I was confident in the material, in the primer that we created, I could never testify to that until I was absolutely certain we had all the conditions down. Bob Brandon: Were you using any other primers? What was your delivery protocol prior to the advent of ZRP? Dr. John Kanca: As you know, I had not done any partial coverages. I had been typically with the zirconia and the modified zirconia, just sand blasting them and cementing them with Resin-Modified Glass Ionomer. With the full crown, at least so far, I haven’t had any trouble with that. This primer now will allow me to do a number of things that I’d been reticent to do before, not the least of which is partial coverage. I think this opens up the door to a lot of things for us and probably for you in terms of the variations in what you can furnish for patients. Bob Brandon: Yes, absolutely. I must say that I’ve seen enough of your preparations. They’re plenty retentive, plenty parallel. I have no doubt the zirconia hasn’t fallen off because of that. Creating the primer for partial coverage particularly, I’m guessing in the posterior, that was the onus of the creation. We do see quite a variety of prep designs, what would almost be three-quarter style posterior preps or onlay preparations with a small pontic like a second bicuspid pontic, and the clinician will state something like, “Well, E.max lasted three years. I want something that is still aesthetic, but is going to last me 10 to 15 years.” We try to mill these out of the KDZ Bruxer aesthetic. Now, we have another arrow in our bag to allow the clinician to bond these in, which is fantastic. Dr. John Kanca: As you know, the Bruxer aesthetic for me has become my go to crown. I see zirconia as the new gold. I think that it’s extremely reliable if you observe certain conditions all the time, not the least of which is you make sure you have two millimeters of occlusal reduction and incisal reduction. If you do that, you’re not going to have any problems. I know some people have a proponents of more conservative preparations. In my opinion, no. If you stick to the two millimeter occlusal reduction, you stay with that, you’re going to be okay. I’ve had no failures to date, but I do stick to that pretty closely. Bob Brandon: I can definitely attest to that fact. Over 90% of the Bruxer or Bruxer aesthetic fractured cases that we received back, we’ll put a caliper or gage on them, and right at the fracture line, we’re always under one millimeter. It’s a limitation of the material. I think the Bruxer first came out as, it’s strong as gold, it’s a gold replacement, you can prep it like gold, but I can’t agree more with your statement on occlusal reduction because we see it back here in the laboratory, we measure our failures, and it’s always what you said there. Dr. John Kanca: Yes, there’s no question in my mind that in clinical practice out there in the world, when you do see a failure like that, it’s going to be from under reduction. The other thing that needs to be stressed is that the central fossa crown preparations needs to be actually more than you think in terms of reduction because people tend to do [inaudible 00:15:24] preparations, table top preparations, flat, and if you try to put anatomy into those flat top preparations, then it’s going to be very thin in the occlusal fossa and the central fossa of those crowns. Bob Brandon: [crosstalk 00:15:42]. Dr. John Kanca: I always tell audiences in lectures that you have to make sure you reduce enough so you have tow millimeters of thickness from the bottom of the proposed anatomy in the tooth in the final crown. Wherever that is, you’re going to have two millimeters underneath that so that you as a lab can design confidently the anatomy like you have, but still have two millimeters underneath it. Bob Brandon: Extremely important and we find that … We’re designing these restorations on a computer. There’s a design software and we can put on a measuring tool for the final restoration thickness. It shows up red any place that’s under two millimeters and it is mainly in the central fossa of these crown designs. These are the cases where we have to call the customer and we’ll say, “I’m sorry, Doctor Jones. Can we reduce a little bit of the upper tooth? I can’t make you a reduction coping in this area because it is a table top preparation and the final restoration won’t fit.” Yes, we’re literally having to reduce the opposing dentition on these cases which you’re just describing. Yes, extremely important point on prep design for the central fossa of these restorations. Dr. John Kanca: This is speaking to a little bit outside the box here for a sec, but the other side of this is that people do need to look at the opposing [inaudible 00:17:10] because if you’re looking at in the posterior, some of these deep cusp relationships and there’s no immediate anterior disclusion, sometimes you do well to reduce whatever the opposing arch is. Reduce the opposing arch somewhat to reduce the depth of that cusp fossa relationship. I don’t hesitate to do that anymore either because not doing so, so frequently results in the fracture of marginal ridges, especially in the second molars and the distal marginal ridges of second molars. It’s one of the flags I tell people to look for all the time. One should not hesitate if there’s any question you see these very deep cusp fossa relationships or you’re doing a crown on a tooth because the second molar distal ridge is fractured or something, then look to the opposing arch and don’t hesitate to reduce the cusp that’s blowing in there. Bob Brandon: I remember when we started back doing your cases in 2004. It was Captek, which was a PFM. Then, we started with some E.max and some Empress. Now, we’ve finally settled on the KDZ Bruxer aesthetic, the high translucent zirconia. We still have an awful lot of PFM customers. We’ve done PFM cases for you. What is your clinical protocol for cementation using the Apex Dental Materials’ lines of product for let’s say a PFM, then a lithium di silicate restoration? Dr. John Kanca: Typically for PFM, to be candid with it, I just use a Resin-Modified Glass Ionomer. My RMGI of choice at this time is Ultra-Cem from Ultradent. They have an auto dispenser that mixes the powder liquid very efficiently and very quickly. We just love that. That is our go to cement for porcelain fused to metal. There are many times that percaline fused metal is realistically the only choice to make. We will do those whenever it’s appropriate, whenever we have to do that. As far as the lithium di silicate, either it comes back from the back either etched with hydrofluoric acid or whatever. If not, if there’s any question, we’ll just sand blast the internal aspect on that because that’s really for the delivery of these restorations, all you need to do is you can hydrofluoric acid etch it if you want, or you can just sand blast it and that’s going to be enough. Then, we would apply interface to the inside, dry it. After it’s mixed, apply it, thin it out, dry it, and then apply a coat of either Surpass Two or Superb. Thinning it out dramatically, and then light activating it. Dr. John Kanca: That differs a little bit from many of the other protocols. However, the application of either Surpass Two or Superb to the unit you’re delivering creates an immediate and very high bond strength once it’s glued into place, so there is no waiting for the generation of a bond over time. You have an immediate bond to the ceramic. That to me has always been very important. The tooth again would be treated with either Surpass or Superb thinned out as much as you can, light activated, and then cemented with, if you’re not in a big hurry, Anchor works really well. Anchor A2 from Apex is a wonderful universal shade for this purpose. If you’re comfortable of the fit and you want something to move along quickly, you can also deliver it with Injectafil with either the A2 or the A4 shade. If you’re using that, you have to be ready, you have to move quickly, and you have to be confident. Again, we’ll get this in the mouth and seat it quickly because that material will being to gel in about a minute. It does speed up your working time and you can get this done efficiently and quickly, but you have to be ready for that. Dr. John Kanca: Then, once the material have gelled, once you clean up the excess, then everything is light activated appropriately for each surface. Now, I’m at a point where I’m using for the most part a high speed or a high energy device, the Valo from Ultradent, to light activate these prosthetics where I am bonding. I use it at typically the highest power setting. Usually, that ends up being about three seconds per surface. That’s where we stand today. Bob Brandon: Do you change your light setting or duration when you move into the zirconias due to the higher level of opacity of the material or even thickness? Dr. John Kanca: When you get into the pure polycrystalline oxides, the Bruxers, it’s very hard to drive light through that. On those, you’re really depending on the dual care nature of these materials and the self care aspect of that dual care nature. In the more translucent, you’re going to be able to get light through them. That’s fine too. Like I said, you may double the cycles, but I think the highest power density setting is appropriate in order to try to drive any light through those materials. Bob Brandon: Yes, I think some of our customers that are using an inferior light source, they really have issues with the zirconia curing and bonding. We see a fairly large number of cases come back that the attempted delivery is unsuccessful and the prescription reads, “Please, clean out all the cement so I can try again.” Dr. John Kanca: If the cement is in the crown, it suggests the failures at the tooth surface, not at the restoration interface. Bob Brandon: Correct. Well, yes. It was a failure at the cementation appointment. By the time with traditional two day shipping, [inaudible 00:23:36] back to us. The cement is very hard and it is adhering to the zirconia. It was either contamination on the tooth surface, was probably the culprit as you said. Dr. John Kanca: Yes. If you’re bonding anything, obviously control of the field is imperative. As I said, you have to be ready, you have to follow protocol, and you got to be ready for these things when you’re inserting them. If you’re going to do that, then it’s going to be okay. We got a lot of feedback before we had created the zirconia primer that crowns were coming off when they attempted to bond them on zirconia crowns. I did warn against that without a good zirconia primer, you’re rolling the dice if you’re attempting to bond these things on because it’s more important than anything is to have that zirconia primer in place if you’re going to attempt to bond them. As long as you have an adhesive that’s capable of sticking to a dual care or self care material and you have the primer, then you can go ahead and do this. It becomes more imperative that you have something, the primer like I said, then follow it with something like Superb or Surpass Two that you can generate, put it in, and light activate that on the crown. You generate immediate bond strengths to that crown and that’ll lessen the possibility that you’ll have it dislodge early. Bob Brandon: Is there anything else you want to add or let our audience know about the ZRP, the primer, how to order it, contact Apex Dental Materials on the website, is it sold through other distributors now? Dr. John Kanca: Well, I’m not sure if you’re aware, but Apex has been acquired by Vista Dental. Bob Brandon: I was aware. Dr. John Kanca: Okay. You can order directly, you can actually order the product through Apex directly, or you can order it through Vista, whichever is handier for you. It can also be ordered on the website. We’re trying to make it as easy as possible. I am presently engaged in looking for an expansion of applications for the material. I would be happy to share that with you when I’m ready to do that. Bob Brandon: Excellent. Dr. John Kanca: In addition if I might, people really want to pay attention to coming events from Apex and Vista because we’ve got some pretty awesome things on the way. I do not exaggerate when I say awesome. Bob Brandon: Are you lecturing again? Dr. John Kanca: I will be lecturing at the Greater New York meeting this year on Friday, the day after Thanksgiving. I will be at the Vista booth for at least a couple days, at least Sunday and Monday for sure, so I will be there. We have some pretty neat things on the way. Bob Brandon: I must say I’ve always enjoyed listening and watching your lectures. The slides you show, especially back when you were creating interface and Surpass where you put the slide up, this is wet, this is dry, and you can’t see a seam, it was truly amazing. I would encourage anybody that’s going to attend the Greater New York, go see Doctor Kanca. It is one hour, two hours, or three hours of the best clinical dentistry that you will ever see. I can’t thank you enough. Doctor Kanca, you’ve done so much for our profession. Thank you for spending this half hour with us, and thank you for continuing to create. There are very few creators and innovators out there. I admire you tremendously for that. Dr. John Kanca: I really appreciate it, Bob. I’m just going to drop one more little thing on you. That is that sometimes, if people need to go through a zirconia crown for the purposes of [inaudible 00:27:56] treatment. Now, we have a way of sealing up those crowns, those access openings as well. It works really well because I did one yesterday. That’s there too, so you can actually use that to bond your crown and close them with composite to the zirconia. I just wanted to mention that. Otherwise, I usually do appreciate everything you’ve said. It’s never unappreciated and never goes by me without appreciation. I thank you for that. Bob Brandon: Thank you so much. I have learned so much from you in the past 15 years just listening to you, seeing your slides. I still remember that one night in San Diego at the AECD, it’s tremendous what you’ve taught me personally over the past 15 years. I can never repay that, but thank you for all of that. Dr. John Kanca: I appreciate that Keating has listened when offered, not for every dumb thing but the things that matter and they’ve always been attentive to that. I do appreciate that as well. Bob Brandon: Thank you so much. Have a wonderful day. Have a great week. Continued success to you, Scott, Chris, and the new partnership with Vista. Thank you so much. Dr. John Kanca: To you as well. Say hi to Shaun for me. Bob Brandon: Absolutely, will do. Take care, Doctor Kanca. Thank you. Dr. John Kanca: Have a good one. Host: Thanks for joining us on the Dental-Up Podcast show this week. Make sure to follow us on Facebook, Instagram, and Twitter, or search the Dental-Up Podcast on iTunes for our weekly feed. Don’t forget to visit KeatingDentalLab.com/promo for exclusive offers. Keating Dental Lab is a full service dental laboratory and we’re nationwide. We’d love for you to send us a case so we can show you the Keating difference. If you dig what you heard, please leave a review on iTunes. We’ll be back next week. [/bg_collapse]